How to Implement Effective Infection Control Measures in a Hospital Setting
Infection control measures are critical in any healthcare setting to prevent the spread of infectious diseases and ensure the safety of patients, healthcare workers, and visitors. In a hospital setting, implementing effective infection control measures is essential to prevent hospital-acquired infections (HAIs) and maintain a safe environment for all those involved.
Why Effective Infection Control is Important
HAIs are a significant concern for hospitals and healthcare facilities worldwide. According to the World Health Organization (WHO), millions of patients are affected by HAIs each year, leading to prolonged hospital stays, increased healthcare costs, and even death. Effective infection control measures can help prevent the spread of HAIs and protect patients and healthcare workers from infection.
Key Elements of Effective Infection Control
Implementing effective infection control measures requires a comprehensive approach that involves multiple key elements, including:
- Hand hygiene
- Personal protective equipment (PPE)
- Cleaning and disinfection
- Isolation precautions
- Environmental controls
By incorporating these elements into infection control policies and procedures, hospitals can create a safe and healthy environment for everyone involved.
Understanding Infection Control
Infection control is the practice of preventing the spread of infections or diseases in healthcare settings. It involves implementing measures to reduce the risk of transmission of infectious agents from one person to another, as well as from the environment to the patient and healthcare workers.
Why is Infection Control Important in a Hospital Setting?
Hospitals are high-risk environments for infections due to the presence of sick patients, healthcare workers, and visitors. Infection control is essential to prevent the spread of infections from one patient to another and to protect healthcare workers from acquiring infections from patients.
Effective infection control measures can help reduce the incidence of healthcare-associated infections (HAIs), which are infections that patients acquire while receiving medical treatment in a healthcare facility. HAIs can lead to prolonged hospital stays, increased morbidity and mortality, and increased healthcare costs.
Furthermore, infection control is crucial in preventing the spread of infectious diseases within the community. Patients who are discharged from the hospital with an infectious disease can potentially spread the disease to their family, friends, and the general public.
Therefore, implementing effective infection control measures in a hospital setting is essential in ensuring the safety of patients, healthcare workers, and the community.
- Some of the essential infection control measures in a hospital setting include:
- Hand hygiene
- Personal protective equipment (PPE)
- Cleaning and disinfection of patient care areas
- Isolation precautions for patients with infectious diseases
- Safe injection practices
- Respiratory hygiene and cough etiquette
- Proper management of medical waste
Effective implementation of these infection control measures can help reduce the risk of transmission of infectious agents and prevent the spread of infections in healthcare settings.
| Benefits of Effective Infection Control Measures |
|---|
| Reduction in the incidence of healthcare-associated infections (HAIs) |
| Improved patient outcomes |
| Reduced healthcare costs |
| Improved safety of healthcare workers and patients |
Key Elements of Effective Infection Control Measures
Effective infection control measures are crucial in preventing the spread of infections in hospital settings. Here are the key elements of implementing effective infection control measures:
Hand Hygiene
Hand hygiene is the most important infection control measure that healthcare workers can take to prevent the spread of infections. Proper hand hygiene involves washing hands with soap and water or using an alcohol-based hand sanitizer before and after patient care, after handling contaminated materials, and after removing gloves. Healthcare workers should also avoid touching their face, mouth, and nose with their hands.
Personal Protective Equipment (PPE)
Personal protective equipment (PPE) includes gloves, gowns, masks, and eye protection. Healthcare workers should wear PPE when caring for patients with infectious diseases or when handling contaminated materials. PPE should be removed and disposed of properly after use.
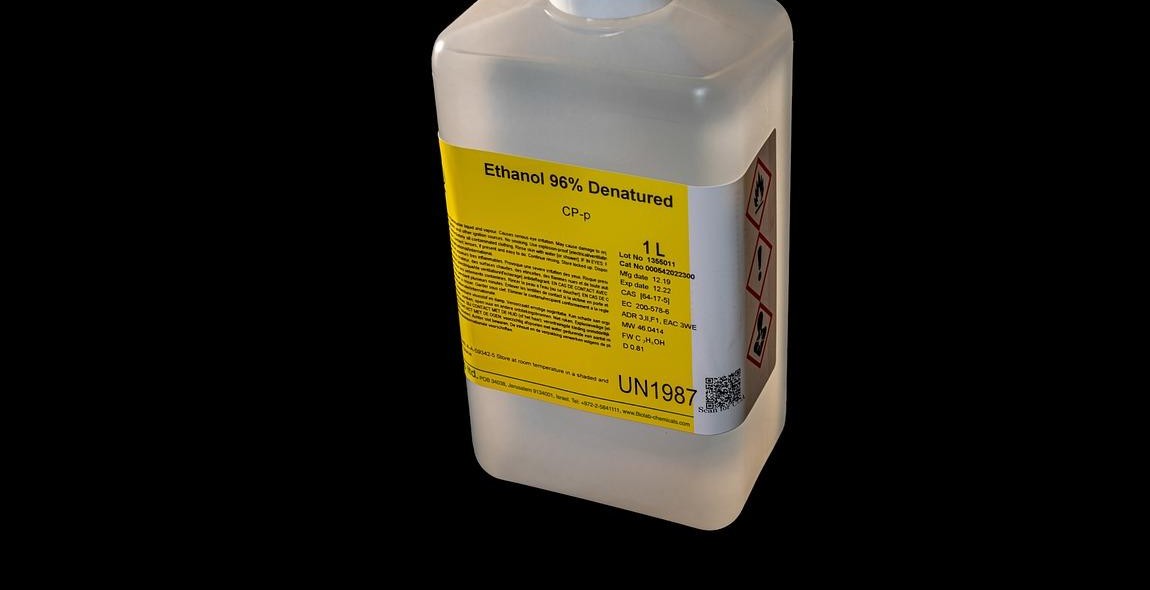
Environmental Cleaning and Disinfection
Environmental cleaning and disinfection are essential in preventing the spread of infections. Surfaces and equipment in patient rooms and other areas should be cleaned and disinfected regularly using appropriate disinfectants.
Isolation Precautions
Isolation precautions are used to prevent the spread of infections from patients with known or suspected infectious diseases. Patients with infectious diseases should be placed in appropriate isolation precautions based on the mode of transmission of the disease.
Patient Placement
Patient placement is an important infection control measure that involves placing patients with infectious diseases in rooms or areas that are appropriate for their condition. Patients with airborne infections should be placed in negative pressure rooms to prevent the spread of the disease to other patients and healthcare workers.
| Key Element | Description |
|---|---|
| Hand Hygiene | Washing hands with soap and water or using an alcohol-based hand sanitizer |
| Personal Protective Equipment (PPE) | Gloves, gowns, masks, and eye protection |
| Environmental Cleaning and Disinfection | Cleaning and disinfecting surfaces and equipment |
| Isolation Precautions | Preventing the spread of infections from patients with known or suspected infectious diseases |
| Patient Placement | Placing patients with infectious diseases in appropriate rooms or areas |

Training and Education
Training and education are crucial components of implementing an effective infection control program in a hospital setting. Proper training can help ensure that staff members understand the importance of infection control measures and know how to properly implement them.
Importance of Training and Education
One of the main reasons why training and education are so important is that they help to prevent the spread of infections. When staff members are properly trained on infection control measures, they are more likely to follow proper procedures and take steps to prevent the spread of germs and bacteria.
Training and education can also help to improve the overall quality of care provided by a hospital. When staff members are trained to properly handle infections, they can help to reduce the risk of complications and improve patient outcomes.
Who Needs to be Trained?
All staff members who work in a hospital setting should be trained on infection control measures. This includes doctors, nurses, support staff, and anyone else who comes into contact with patients or handles medical equipment.
What Should be Included in Training?
Training on infection control measures should cover a wide range of topics, including:
- The importance of hand hygiene
- The proper use of personal protective equipment (PPE)
- The proper cleaning and disinfection of medical equipment and surfaces
- How to safely handle and dispose of contaminated materials
- The signs and symptoms of common infections
Training should also be ongoing, with regular updates and refresher courses to ensure that staff members stay up-to-date on the latest infection control guidelines and best practices.
| Training Topic | Description |
|---|---|
| Hand hygiene | Proper handwashing techniques, use of hand sanitizer, etc. |
| Personal protective equipment (PPE) | When and how to use PPE, proper disposal, etc. |
| Cleaning and disinfection | Proper techniques for cleaning and disinfecting medical equipment and surfaces |
| Safe handling and disposal | How to safely handle and dispose of contaminated materials, including sharps |
| Infection awareness | Signs and symptoms of common infections, how to prevent their spread |
Monitoring and Evaluation
Monitoring and evaluation (M&E) is an essential component of implementing effective infection control measures in a hospital setting. It involves tracking and assessing the progress and effectiveness of infection control measures over time.
Why is Monitoring and Evaluation Important?
Monitoring and evaluation is important because it allows healthcare providers to:
- Identify areas of weakness in infection control measures and improve them
- Ensure that infection control measures are being implemented correctly and consistently
- Determine the effectiveness of infection control measures in preventing the spread of infections
- Provide data to support decision-making and resource allocation for infection control efforts
What Should be Monitored and Evaluated?
The following aspects of infection control measures should be monitored and evaluated:
- Adherence to hand hygiene protocols
- Use of personal protective equipment (PPE) by healthcare workers
- Cleaning and disinfection of patient rooms, equipment, and other surfaces
- Compliance with isolation precautions for patients with infectious diseases
- Rates of healthcare-associated infections (HAIs)
How Should Monitoring and Evaluation be Conducted?
Monitoring and evaluation should be conducted using a combination of methods, including:
- Direct observation of healthcare workers
- Surveys and questionnaires to assess knowledge and attitudes towards infection control
- Review of medical records and infection control data
- Environmental sampling to assess the presence of pathogens on surfaces
The data collected through monitoring and evaluation should be analyzed regularly and used to inform decision-making and quality improvement efforts.
Conclusion
Implementing effective infection control measures is crucial in a hospital setting to prevent the spread of deadly diseases and infections. Hospitals must take a proactive approach to prevent the transmission of diseases by following strict guidelines and protocols.
One of the most critical steps in infection control is proper hand hygiene. Healthcare workers must wash their hands frequently and use hand sanitizers to prevent the spread of infections. Additionally, hospitals must ensure that their cleaning and disinfection protocols are up-to-date and effective.
Personal protective equipment (PPE) such as gloves, gowns, and masks must be used appropriately to prevent the spread of infections. Patients with contagious diseases should be isolated, and healthcare workers must wear appropriate PPE when treating them.
Education and training of healthcare workers are also essential in preventing the spread of infections. Hospitals must provide regular training sessions to their staff to ensure that they are aware of the latest infection control guidelines and protocols.
Overall, implementing effective infection control measures in a hospital setting requires a collaborative effort from all healthcare workers, patients, and visitors. By following strict guidelines and protocols, hospitals can prevent the spread of deadly diseases and infections, ensuring the safety and well-being of everyone involved.
